The role of estrogen type in the establishment and mediation of endometriosis:
Main point: "...We find, as shown previously (42–44), that estradiol is not required for establishment of endometriosis-like lesions.... Finally, endometriosis-like lesion growth is mediated predominately by estradiol signaling via ERα to increase lesion size, fluid volume, increased epithelial cell height, and epithelial cell proliferation...." http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3404357/
So what does that mean? Get a snack and get comfy.
First a little basic background on estrogen receptors and what they do and do not do:
(Cute, isn't it?)
So your cells have a protein in them called estrogen receptors (ER) that are activated by estrogen. These receptors just hang out in your nucleus waiting for something to happen- ready for some action. When they meet up with estrogen- game on! Once activated, the ER finds its way to your DNA and it controls how your DNA is read & transcribed.
"Estrogens are made in the ovaries and then delivered within seconds throughout the body in the blood...Estrogens pass directly into cells throughout the body, so the cell can use receptors that are in the nucleus, right at the site of action on the DNA. When estrogen enters the nucleus, it binds to the estrogen receptor, causing it to pair up and form a dimer. This dimer then binds to several dozen specific sites in the DNA, strategically placed next to the genes that need to be activated. Then, the DNA-bound receptor activates the DNA-reading machinery and starts the production of messenger RNA." http://www.rcsb.org/pdb/101/motm.do?momID=45
So estrogen binds to your estrogen receptors (like a key & a lock) and starts your genes to workin':
It "reads" your DNA and starts copying portions of it to make your cells do certain stuff.
You have several sites for estrogen receptors:
(more on ERα and ERβ later)
Gene expression is the way your body takes part of your DNA and uses that to make materials(a "gene product"- mostly proteins) that affect how your body works. If something goes wrong with this process- watch out! Trouble!
So, estrogen can do a lot of good stuff for your body:
But how does estrogen affect endometriosis? The search continues.....
"Estrogens influence many physiological processes in mammals, including but not limited to reproduction, cardiovascular health, bone integrity, cognition, and behavior. Given this widespread role for estrogen in human physiology, it is not surprising that estrogen is also implicated in the development or progression of numerous diseases, which include but are not limited to various types of cancer (breast, ovarian, colorectal, prostate, endometrial), osteoporosis, neurodegenerative diseases, cardiovascular disease, insulin resistance, lupus erythematosus, endometriosis, and obesity. In many of these diseases, estrogen mediates its effects through the estrogen receptor (ER), which serves as the basis for many therapeutic interventions....Finally, diseases exist for which estrogen has been implicated in their pathogenesis but a definitive role for the ER has yet to be established. These include endometriosis and polycystic ovary syndrome,...What role the ER may play in the risk or severity of these and other diseases will no doubt increase our ever-expanding knowledge of the relationship among estrogen, ERs, and disease." http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2373424/
Now these receptors don't do it all by themselves. Other stuff comes into play. Now maybe it's time to take a look at just what estrogen does to your uterus and what other hormones come into play with a woman's cycle. This explains it pretty well:
"Hormones are chemicals that are made in small organs called glands. Hormones move about the body, usually through the bloodstream, and change or regulate the function of other organs and structures. In effect, the release of hormones is one of the ways that different parts of the body communicate with each other. The hormones we are most concerned about here are estrogen, progesterone, and testosterone....
"The ovaries make estrogen and progesterone, as well as various other hormones, in a cyclic fashion, and the levels of these hormones rise and fall with ovulation. For most women, this will be a monthly cycle, interrupted now and then by pregnancy or disrupted by stressful events....Thought of as the primary female hormone, estrogen builds up the uterine lining, stimulates breast tissue, and thickens the vaginal wall. It also affects almost every other organ in the body. Estrogen plays a critical role in bone building and is thought to have important protective effects on the cardiovascular system.
Progesterone, which is made only during the second half of the menstrual cycle, prepares the uterine lining for an egg to implant, but progesterone also has other important effects on many of the tissues sensitive to estrogen. Testosterone, also made in the ovaries, plays a role in stimulating sexual desire, generating energy, and developing muscle mass.
The balance of hormones in your body at any given point is affected by many factors. The pituitary gland, at the base of your brain, and your ovaries are constantly communicating via their respective hormones, dictating the changing hormone levels of your monthly cycle and the production of eggs. The pituitary produces follicle-stimulating hormone and other hormones. Stress, body weight, time of day, time of the month, and any medications you take can all cause temporary changes in your hormone levels." http://health.howstuffworks.com/wellness/women/menopause/how-menopause-works2.htm
So your hormones should cycle something like this:
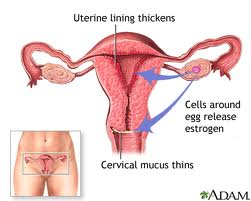
And when estrogen is high, it makes the uterine wall thicken (gotta get ready in case of baby!):
So what role, exactly do estrogen and its receptors play in endometriosis?
"Estrogen signaling is a balance between two opposing forces in the form of two distinct receptors (ER alpha and ER beta) and their splice variants. We have also become aware that ERs do not function by themselves but require a number of coregulatory proteins whose cell-specific expression explains some of the distinct cellular actions of estrogen. Estrogen is an important morphogen, and many of its proliferative effects on the epithelial compartment of glands are mediated by growth factors secreted from the stromal compartment. Thus understanding the cross-talk between growth factor and estrogen signaling is essential for understanding both normal and malignant growth." http://www.ncbi.nlm.nih.gov/pubmed/17615392
"...We find, as shown previously (42–44), that estradiol is not required for establishment of endometriosis-like lesions.... Finally, endometriosis-like lesion growth is mediated predominately by estradiol signaling via ERα to increase lesion size, fluid volume, increased epithelial cell height, and epithelial cell proliferation...." http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3404357/
"Using a mouse model of endometriosis, we demonstrate the importance of ERα and ERβ activity and estradiol-mediated signaling in multiple components of the development of endometriosis-like lesions.... We find, as shown previously (42–44), that estradiol is not required for establishment of endometriosis-like lesions.... These findings suggest the important role of paracrine-mediated responses in lesion responsiveness. Finally, endometriosis-like lesion growth is mediated predominately by estradiol signaling via ERα to increase lesion size, fluid volume, increased epithelial cell height, and epithelial cell proliferation.... Our results demonstrate the important role for the host estradiol, ERα-mediated signaling on lesion responsiveness. The effects of estradiol are dependent on multiple criteria including the immune stimulus, the cell types involved during different phases of disease, the amount of estradiol, and the microenvironment (26). The roles of estradiol on inflammation and neoangiogenesis via ERα oppose each other in endometriosis, and this is seen in our model system. The WT to WT estradiol group, having increased mitogenesis and a decrease in inflammation results in larger, cystic, proliferative lesions. This opposing role of estradiol in this model and in women with endometriosis requires in-depth focus on the mechanistic actions of ERα for the development of selective ER modulators that will allow for the uncoupling of these mechanisms of action to focus efforts for disease treatment." Full article here: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3404357/
So, to sum it up, the estrogen receptor alpha relates to how the endo lesions grow. When using treatments to lower the estrogen in your body, you're essentially trying to lower amount of activation that the ERα receives. By doing that, you are hopefully controlling the endo lesions' size, fluid volume, increased epithelial cell height, and epithelial cell proliferation. But in doing so though, you also affect your central nervous system, cardiovascular system, liver, breasts, gastrointestinal tract, and bones (which accounts for the side effects of medications like GnRH, etc). With excision, you are removing the lesions themselves. But the question stills remains, how do endometrial lesions get there in the first place? If you remove them, can more arise? More research needs to be done, but most theories support stem cell involvement:
"The pathogenesis of endometriosis is likely multifactorial, and extensive investigation has explored the role of genetics, environmental factors, and the immune system in predisposing patients to developing endometriosis. A series of recent publications have described the identification of endometrial stem/progenitor cells....The origin of endometriotic implants and the pathogenesis of endometriosis has long been an area of active investigation. Multiple hypotheses have been explored, including retrograde menstruation, coelomic metaplasia, embryonic rest theory, and the lymphovascular metastasis theory.... the data suggest that endometrial stem/progenitor cells function in the development of endometriosis. Additionally, bone marrow–derived stem cells can target the uterus and differentiate into a functional endometrium and, experimentally, extrauterine stem cells can target endometriotic implants. Furthermore, the contribution of stem/progenitor cells to the pathogenesis of endometriosis could account for the observations that drive all theories of the cellular origin of ectopic endometriotic implants. Endometrium-derived stem/progenitor cells residing in the basalis layer can be shed through the fallopian tube to establish endometriotic implants, accounting for the findings that support the retrograde menstruation theory. Stem/progenitor cells derived from either the bone marrow, the endometrium, or an alternate source may be responsible for the observations that support the theory of coelomic metaplasia. Potential stem/progenitor cells that persist in the remnants of the mullerian system can form endometriotic implants and account for the embryonic rest theory. Finally, extrauterine stem/progenitor cells, derived from the bone marrow or an alternative source, are likely to travel to distant ectopic sites via the lymphovascular spaces." http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3107843/
Does your head hurt now? Mine does! Some days it's interesting to study this, other days all I know is:
I like how Dean Ornish put it when it goes to science and healing:
Not have enough yet? Want to read on about food and estrogen? You glutton for punishment!! Here ya go:
"To date, research has shown that promoting the growth of certain beneficial intestinal microorganisms can help to improve overall health. 'In this study, we wanted to determine if steroid hormone nuclear receptors, specifically estrogen receptor beta, affect the composition of intestinal bacteria,' said Dr. Joseph Sturino....Some steroid hormones, like estradiol, and dietary phytoestrogens are known to influence the development of chronic gastrointestinal inflammation and estrogen-responsive cancers of the breast, prostate and colon," Sturino said. Some of these effects are the result of differential and tissue-specific gene regulation by estrogen receptor beta...'Interestingly, however, we also found that the microorganisms differed between mice that expressed estrogen receptor beta and those that did not.' Distinct patterns for Lactobacillales were exclusive to and highly abundant among mice fed a complex diet containing isoflavones, Sturino explained. 'Some Lactobacillales have probiotic function when taken in adequate numbers in food or dietary supplements, so indigenous species might also act to promote gut health,' he said." http://www.sciencedaily.com/releases/2013/11/131108124854.htm
In other words, mice while eating a plant based (isoflavone rich) diet had more good bacteria to help regulate GI and immune function; but, when they switched to a diet high in refined sugars, they had more bad bacteria (think E coli and salmonella).
Different Nutrients and Their Effect On Estrogen:
Folate - Deficiency reduces estrogen levels; Excess folate is linked to some types of estrogen-related breast cancer; Detoxifies excess estrogen via methylation pathway; Regulates estrogen’s effect on genes.1,2,3
Vitamin B6 - Protects genes from estrogen-induced damage thus lowering risk of hormone related cancers; Detoxifies excess estrogen via methylation pathway; Estrogen-based oral contraceptives cause B6 deficiency.4,5,6,7
Vitamin D - Regulates synthesis of estradiol and estrone; Enhances estrogen’s protective effect on bones.8,9,10
Vitamin C - Increases the most potent estrogen (estradiol) in women on hormone therapy; Lowers aromatase (enzyme that converts testosterone to estrogen) in ovaries.11.12.13
Vitamin K - Inhibits estrogen activity by binding to estrogen receptors; Lowers the ratio of estradiol (strong estrogen) to estrone (weaker estrogen).14,15
Vitamin E - Deficiency impairs estrogen detoxification pathway; Some forms of vitamin E inhibit estrogen action, especially in breast tissue; Low levels linked to higher estrogen.1,16,17
Vitamin A - Helps metabolize the biologically active estrogen (estradiol) to an inactive form (estrone).18,19
Calcium - Calcium-D-glucarate lowers estradiol levels; Helps breakdown estrogen in the liver and convert it to a less toxic form.1,20,21
Selenium - Estrogen levels affect how selenium is distributed to various tissues in the body.22,23
Magnesium - Cofactor for the enzyme that removes toxic forms of estrogen (catechol-O-methyltransferase); Estrogen alters magnesium levels throughout menstrual cycle.1,24,25,26
Zinc - Estrogen lowers risk of zinc deficiency; Zinc dependent proteins metabolize estrogen.26,27,28
Cysteine - Prevents oxidation of estrogen into a dangerous form that causes breast cancer.29,30,31
Dietary estrogens and estrogen receptors:
"In this month’s issue, Georgi N. Nikov of Tulane University in New Orleans, Louisiana, and colleagues examine the activity of dietary estrogens in humans.
They confirm that
dietary estrogens have different affinities for human estrogen receptors.
They also found that, once bound, each estrogen can also alter a receptor’s shape and size.
When estrogen binds to a receptor, the resulting complex interacts with a site within a target gene’s regulatory region. That interaction may either promote or inhibit gene transcription. Alterations in the receptor’s shape may affect how well the estrogen receptor complex can initiate or inhibit gene transcription. Nikov and his colleagues focused on four phytoestrogens—genistein, coumestrol, daidzein, and glyceollin—and the mycoestrogen zearalenone. Genistein and daidzein are normal components of soybeans, which also produce glyceollin when subjected to certain stresses.
Coumestrol is produced by clover, and zearalenone is generated by
Fusarium molds, which infect grains.
The team first measured the estrogens’ affinities for two estrogen
receptors, ERα and ER (beta), as compared to estradiol, the form of estrogen
normally found in the body. But knowing that an estrogen binds
to a receptor is only half the story; what follows is perhaps even moreimportant. Therefore, the researchers also investigated how receptor
complexes interact with estrogen response element (ERE) sequences,
regulatory sites that turn genes off or on....
The researchers found that, except for glyceollin, all ofthe tested estrogens had a greater affinity for ER (beta) than
ERα; glyceollin had the opposite preference. However,
the glyceollin–receptor complexes, unlike the other complexes,
did not interact with either ERE sequence. The
interactions that did occur varied according to the specific
estrogen and which receptor and ERE sequence
were involved; however, none were stronger than those
involving estradiol.
The researchers concluded that just knowing the affinity
of the estrogen for the receptor is not enough. Equally important isthe way the estrogen–receptor complexes interact with ERE
sequences. These interactions may in turn affect transcription of target
genes and thus affect the myriad functions of estrogen in the body.–Julia R. Barrett"
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2556941/